It was the worst news two prospective parents could get. As described in the New York Post, Shelley and Rob Wall were told their baby had “no brain.” Doctors believed it had not developed. The couple, from Cumbria, in northwest England, were advised on multiple occasions to terminate the pregnancy. They were told their child would never see, hear, eat, or talk. However, they refused to give up hope. On 11/11, at 11 o’clock, little Noah was born.
Six years later, he had made remarkable progress. He was a bright, interactive child who could certainly see, hear, eat, and talk. Thanks to intensive physical therapy he was learning to walk, and even to surf. Noah had gone from having an estimated 2% of a normal brain size at birth to a brain size that was 80% normal at age 6. How is this possible?
Water in the Head
Noah was diagnosed with two conditions, hydrocephalus and spina bifida, that often go together. Let’s start with the first one. Hydrocephalus, which literally means “water in the head,” is an abnormal, increased amount of cerebrospinal fluid within the brain’s deep cavities. (Source: American Association of Neurological Surgeons: Hydrocephalus; Hydrocephalus Association)
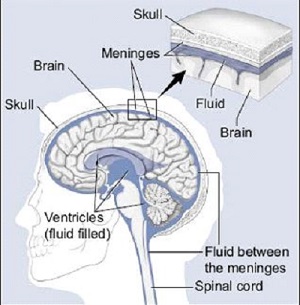
Cerebrospinal fluid, or CSF, is a colorless fluid that flows around and within the brain and spinal cord. CSF cushions the brain, delivers nutrients to brain and spinal cells, and removes waste. CSF is also very important in determining the pressure within the brain. Too much CSF could lead to high pressure in the head, whereas too little CSF could result in low pressure. Within the brain are large CSF-filled cavities called ventricles that communicate with the CSF flowing along the outside of the brain. (Source: American Association of Neurological Surgeons: Hydrocephalus)
Source: University of Miami Health System
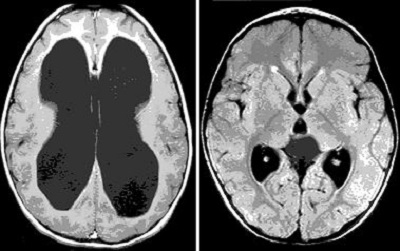
When a person has hydrocephalus these ventricles become distended with fluid, putting pressure on the brain all around them. The following brain MRI shows a brain with hydrocephalus on the left and a normal brain on the right. CSF is black and brain tissue is gray. We are looking at a cross-section of the brain, as though a person were lying down with their feet facing us. Note the large fluid-distended ventricles and the thinned-out brain tissue on the side with hydrocephalus.
Source: Seattle Children’s: Hydrocephalus
It would be easy to assume that the individual on the left does not have as much brain tissue as the individual on the right, but that’s not the case – the brain tissue on the left is just compressed by the fluid-distended ventricles. This is probably what happened with little Noah Wall – his brain was there all along, but it was severely compressed by hydrocephalus.
Before getting into how Noah’s hydrocephalus was likely treated, let’s explore this disorder a little bit more. Hydrocephalus can happen to anyone, but it disproportionately affects infants and those over 60 (Source: American Association of Neurological Surgeons: Hydrocephalus). The Hydrocephalus Association estimates that 1-2 per 1000 babies are born with this condition.
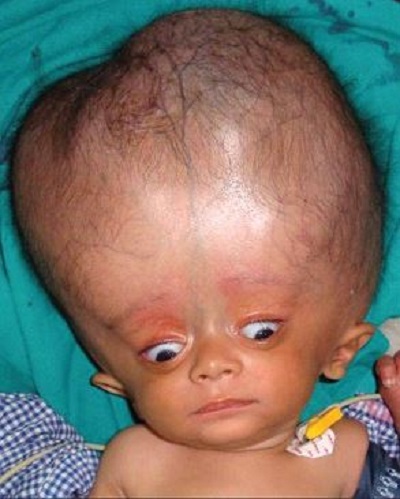
Hydrocephalus can be a complication of premature birth, the result of a developmental disorder like spina bifida, or due to tumors, head injuries, or infections like meningitis. In babies the symptoms of hydrocephalus can include a tense soft spot on the head, poor appetite, vomiting, irritability, sleepiness, eyes turned downward, and prominent veins in the scalp. Other symptoms are related to the fact that the bones in a baby’s head haven’t fused together yet.
A baby’s scalp can look thin, the bones in the baby’s head can appear separated, and the head can even become abnormally enlarged. (Source: American Association of Neurological Surgeons: Hydrocephalus)
Source: Rath G and Dash H. Anaesthesia for neurosurgical procedures in paediatric patients. Indian J Anesth. 56(5):502-510.
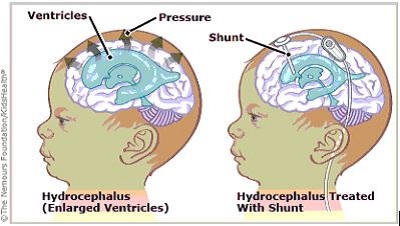
So how is hydrocephalus treated? Sometimes a tumor can be removed and thereby restore the normal flow of CSF. But much of the time the abnormal accumulation of fluid needs to be diverted from the ventricles to another body cavity. Neurosurgeons use a device called a shunt to do this. The commonly used ventriculoperitoneal shunt drains fluid from the ventricles through a tube and into the peritoneal membrane of the abdomen, which absorbs it. (Source: American Association of Neurological Surgeons: Hydrocephalus)
Source: KidsHealth from Nemours
Let’s get back to Noah Wall. He was born with hydrocephalus as a developmental disorder, part of spina bifida. We understand that he probably wasn’t actually missing 98% of his brain – it was probably just really compressed by the CSF filling his ventricles. After Noah was born, doctors inserted a shunt, which drained the excess fluid. Gradually his brain was able to expand to a more normal size, and Noah was able to get on with his life.
Spina Bifida
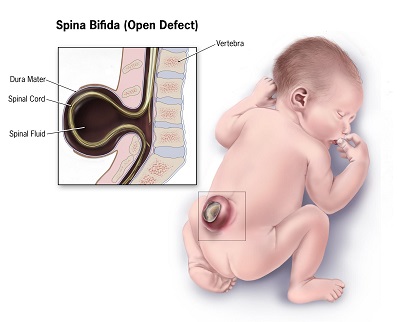
The story doesn’t end here. Noah faces additional challenges because of his diagnosis of spina bifida. Spina bifida refers to a set of congenital conditions in which there is an opening in the spine.
There are three common types of spina bifida:
Spina bifida occulta – “Occulta” means hidden. Here there is an opening in the spine, but no protruding sac or opening in the baby’s back, and the spinal cord and nerves are typically normal.
Meningocele – Here a sac of fluid protrudes through an opening in the baby’s back; it does not contain the spinal cord. There is generally minimal to no nerve damage.
Myelomeningocele – Here a sac of fluid containing part of the spinal cord and nerves protrudes through the baby’s back. In this most severe form, the spinal cord and nerves may be damaged, causing loss of sensation and movement in the legs and feet, and problems with using the bathroom. (Source: CDC Spina Bifida Homepage)
1 in 3000 live births have myelomeningocele. (Source: American College of Obstetricians and Gynecologists Committee Opinion: Maternal-Fetal Surgery for Myelomeningocele)
Source: Mayo Clinic: Spina Bifida
Surgery Before Birth
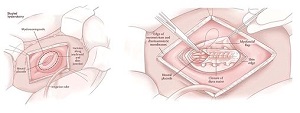
Babies with myelomeningocele (MMC) experience progressive spinal cord damage while they are developing in their mothers. In the past babies’ MMCs were surgically repaired only after delivery. Now, pioneering fetal surgery programs have developed procedures to repair MMCs while fetuses are still developing inside their mothers. Highly trained fetal surgeons can open a woman’s uterus, operate on the baby, and close back up so the pregnancy can proceed as normal. (Source: Children’s Hospital of Philadelphia: About Fetal Surgery for Spina Bifida (Myelomeningocele))
A study found that when compared with surgery after birth, fetal repair of MMC was associated with decreased rate of death and need for a shunt at age 12 months, twice the likelihood of being able to walk at age 30 months, better motor function at age 30 months, and better than expected level of function based on the location of the MMC. The surgery also decrease the risk of hindbrain herniation, in which the lower part of the brain (including the brainstem) sinks downward toward the spinal cord, often causing significant damage. (Source: American College of Obstetricians and Gynecologists Committee Opinion: Maternal-Fetal Surgery for Myelomeningocele)
However, the surgery also has significant risks for mother and baby, so each case must be carefully selected before such surgery is undertaken. (Source: American College of Obstetricians and Gynecologists Committee Opinion: Maternal Fetal Surgery for Myelomeningocele)
Source: Children’s Hospital of Philadelphia: About Fetal Surgery for Spina Bifida (Myelomeningocele)