Epidemiologist MoNique Gaines-Harris responds to fascinating questions on COVID-19.
Note: This article does not cover questions on any variants recently discovered.
Gauze masks were recommended to halt the spread of the Spanish Flu
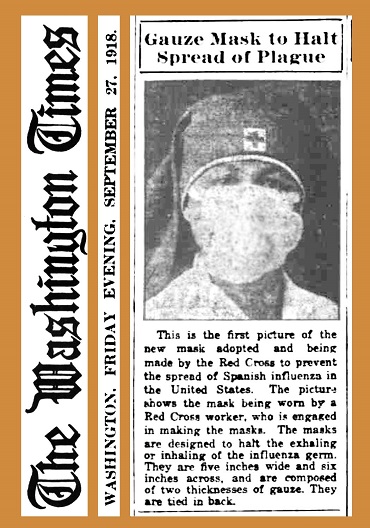
This is a photo from a newspaper article in The Washington Times (September 27, 1918). It shows a woman wearing a gauze mask, which was recommended by Red Cross to help control the spread of the 1918 flu pandemic.
1. Do you think there may be long term effects for asymptomatic coronavirus patients?
There is still a great deal to learn about SARS-CoV-2, even more so concerning asymptomatic individuals. Current studies show radiologic and laboratory findings of some asymptomatic patients are similar to those of symptomatic patients. Specifically, abnormally low white blood cell and platelet counts have been found as well as ground-glass opacities (a white-flecked pattern seen on lung CT scans, indicative of increased density).
Relatively little research has been conducted on long-term symptoms experienced by asymptomatic patients. However, early reports of patients dealing with long-term fatigue, headaches, vertigo, difficulties with cognition, hair loss, cardiac issues, and diminished cardiorespiratory fitness have been identified.
Cell damage that extends beyond the lungs is a common finding with COVID-19. Asymptomatic individuals do not appear immune to internal cellular damage associated with COVD-19. Therefore, until additional research is conducted, it is safe to assume chronic issues are possible for asymptomatic coronavirus patients.
2. Since the coronavirus can enter the eyes, do you think more people will start wearing eye protection in public?
Few studies have been done on the ocular route of transmission for COVID-19. The studies that were conducted included small sample sizes and may not be reflective of the general population.
As with other mucus membranes such as those in the nose and mouth, direct viral contact with mucus membranes in the eye is a possible transmission route for COVID-19. It is impossible to determine the exact portal of entry; however, low viral levels have been found in tears. Studies have shown ophthalmic manifestations of COVID-19 with the first symptom of disease involving the eye.
Despite these findings, there is no evidence to suggest the general public will begin wearing eye protection as a means of protecting themselves from COVID-19.
I would not recommend using eye protection for the general public as ocular transmission is thought to be extremely rare. If social distancing guidelines are followed, the distance between individuals should be sufficient to mitigate the risk. Furthermore, eye protection would increase the number of times a person needs to touch their face, thereby increasing transmission risk.
3. Can I get COVID-19 from sexual intercourse?
The virus has been detected at low levels in semen and was recently detected in the vaginal secretions of a 65-year-old woman. The current consensus is COVID-19 is not transmitted by sexual intercourse itself. However, the close proximity required during times of intimacy puts an individual at risk of encountering respiratory droplets from their partner and coming into contact with other bodily fluids where the virus has been identified, such as feces, urine, and blood.
The guidelines and recommendations for COVID-19 change daily. With the virus recently identified in vaginal secretions, future guidelines may list sexual intercourse as a transmission mode. As we currently stand, no, you cannot contract COVID-19 from sexual intercourse itself. However, the nonadherence to social distancing guidelines during times of intimacy increases the risk of transmission.
4. Is reinfection possible with COVID-19?
This is a question on the mind of scientists as well as the general public. Is reinfection possible? Early studies conducted on rhesus monkeys would suggest reinfections with the same strain of COVID-19 is not possible. However, there has since been at least two cases where reinfection with COVID-19 has occurred. One patient being reinfected just 48 days after primary infection, and the other testing positive 142 days after primary infection.
A study on the Clinical and Immunological Assessment of Asymptomatic SARS-CoV-2 infections noted decreased neutralizing antibodies within 2-3 months after infection. This calls into question the level of protection provided during primary infection, especially since primary infection with other coronaviruses has resulted in high levels of protective antibodies for periods of 24-34 months.
One or two patients are not sufficient to accurately gauge the level of protection provided by primary infection with COVID-19. Nevertheless, they provide data adequate to support the claim that reinfection with COVID-19 is possible, and active immunity may not be our saving grace after all.







